We are currently conducting several studies on different aspects of depression and suicide risk. Read more about our currently active studies below:

Project Lead: Dr. Sakina Rizvi
The prevalence of suicide attempt among individuals with Major Depressive Disorder (MDD) is about 20%. Risk for suicide attempt can be increased by many things such as negative life events, genetics, and changes in the way the body and brain function. It is most likely caused by a combination of several of these factors. Currently, we are conducting a study to identify biological risk factors for suicide attempt. Participation will involve multiple visits completing questionnaires about your mood, performing attention tests, and receiving brain imaging.
Please see the flyer for more information or contact Hailey at [email protected].
Project Lead: Dr. Katharine Dunlop
The prevalence of suicide attempt in Major Depressive Disorder is about 20%. Risk for suicide attempt can be increased by many things such as negative life events, genetics, and changes in the way the body and brain function, and unfortunately we do not have reliable markers that predict an increased suicide risk. In this study, we will be collecting detailed information about participants’ psychiatric history and depression symptoms, as well as brain scans, over a single research visit. Our goal is to use this information to help us determine what best predicts suicide attempt history.
Please see the flyer for more information or contact Dr. Dunlop at [email protected].

Project leads: Drs. Sakina Rizvi, Yvonne Bergmans, and Amanda Ceniti
There is an immense lack of resources available for the friends/family of people experiencing suicide-related thoughts and/or behaviours. To address this gap, the study team aims to (1) conduct an extensive needs assessment across Canada to understand the gaps in support experienced by family/friends and people with lived experience of suicide risk, and (2) use these findings to design a novel suicide prevention training program – the FIRST Program – that is specifically tailored to the needs of friends and family.
We are currently recruiting people across Canada aged 18+ who identify with one or more of the following groups: (1) people who experience suicidal thoughts, (2) people with a history of one or more suicide attempts, (3) people who are supporting/have supported a loved one at risk of suicide, and (4) people impacted by suicide loss (1 year or more following the loss). Participation involves a brief phone screening and a single one-on-one interview conducted virtually.
Please see the flyer for more information or contact the study team at [email protected].
Note: recruitment for this project is currently on pause until 2025.
Project lead: Dr. Sakina Rizvi
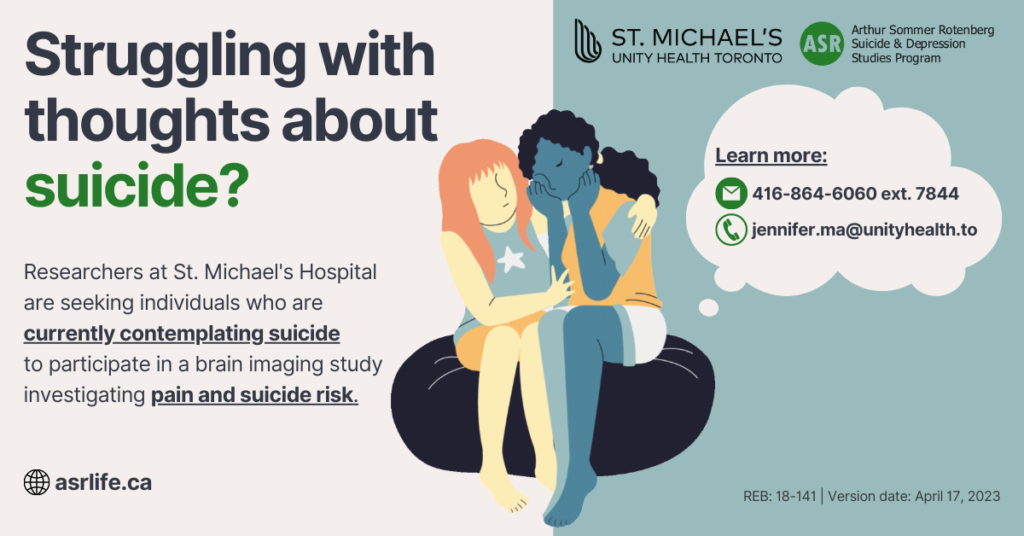
Currently, little evidence exists that tells us how individuals with suicidal ideation differ from those at risk for suicide attempt, illustrating the need for more biomarkers (biological features, i.e.: gene, protein) to guide treatment approach and identify new treatment avenues. This study seeks to investigate the relationship between the brain’s pain perception system and suicidality, in order to identify potential predictors of suicide risk. Participation involves completion of questionnaires, tasks measuring attention, memory and reward, & a brain scan.
We are currently recruiting people aged 18-70 who meet criteria for one the following groups:
(1) individuals with no psychiatric history (i.e. healthy controls). For more information, see the flyer here.
(2) individuals currently contemplating suicide. For more information, see the flyer here.
For more information, see the flyers linked above or contact Jennifer at Jennifer[email protected]
2. Effect of suicidality on social cognition